The COVID-19 pandemic is now a global fact. It still involves many uncertainties. At present and in the near future, we need to handle the ongoing pandemic as a global catastrophic crisis with complex cascading impacts. We also need to start thinking about reconstruction. We are here concerned with reconstruction that will allow polities to fully function again, i.e. not to be in emergency mode. That may go from norms to socio-political systems, through ways to produce goods and services. It may be elements of these systems, or larger parts of them.
In this article, we explain first that we have tools to plan ahead properly and constructively even considering the condition of utter uncertainty. We must not allow the unpreparedness disaster that is also striking us to go on. Unpreparedness, resulting from lack of anticipation, must also stop.
We then turn to the real issue we need to consider: surviving and reconstructing. We thus outline our research question and our scope. We explain that we are coming back to the fundamentals of politics (and not politician politics). We start outlining how both surviving and reconstructing are intertwined. As a result, we paint a sketch of what is ahead and what we need to further research.
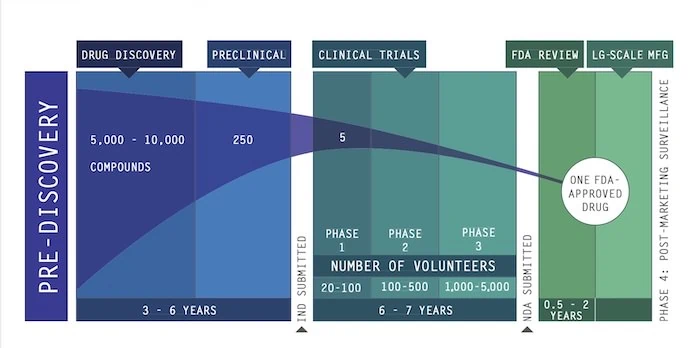
Finally, we start the construction of a structure for our set of scenarios that will outline the possible futures. We underline that two factors are critical and will determine our future: vaccine and antiviral prophylaxis and treatment. Here we focus on the first of this factor, vaccine. We do not only look at the discovery of the right vaccine for the COVID-19 but also at the various stages of the immunization process. As a result, we obtain a first estimate that mass campaigns of vaccination may start earliest around winter 2022-2023 (all vaccine candidates). The next article focuses on antiviral prophylaxis and treatment.
Considering the very large scope of the task ahead, this article is the first of a series of articles focusing on strategic foresight and anticipation to survive at best the COVID-19 and then reconstruct.
To be able to achieve the goals of surviving (across domains) and reconstructing, we need to deploy and use, at the same time, monitoring for warning and strategic foresight. And this is NOT an option but a crucial necessity.
Monitoring for adequate models and to struggle against deadly biases
Monitoring must take place in two areas. First, we must monitor what is happening in science, across many disciplines. Then, we must also consider what is happening on the ground. This monitoring will allow revising a knowledge that is everyday checked, changed, and improved.
With the result of our monitoring, we shall need to update all our models, including those implicit models we use everyday and which are active, unknowingly, in our heads. Indeed, if we do not do that, these inner models will become cognitive biases. And cognitive biases, when survival is at stake, can be deadly.
This part is extremely challenging because we know that human beings are naturally bad at updating the inner models that allow them to understand the world (e.g. Heuer, Richards J. Jr., Psychology of Intelligence Analysis, Center for the Study of Intelligence, Central Intelligence Agency, 1999 – more in our online course 1 – Module 3).
For example, as shown by Anderson et al., if we are presented with a new problem and do not have a lot of information about it, our brain creates a first very approximative model. That model makes sense of whatever data we have (Craig A. Anderson, Mark R. Lepper, and Lee Ross, Perseverance of Social Theories: The Role of Explanation in the Persistence of Discredited Information, Journal of Personality and Social Psychology 1980, Vol. 39, No.6, 1037-1049).
Then, once this model is created, it becomes very difficult to change it. Effort is necessary to do so. In other words, most people, will stick to their initial model, even though new facts and evidence arise. It is not that they lie or that they show bad will, although this, of course, may also happen. It is that those people had first to make sense of a new problem with insufficient information. As they receive new information, their model has become inadequate but it still filters their understanding (Craig A. Anderson et al. ibid.).
Unfortunately, the COVID-19 pandemic exactly corresponds to the worst possible case to generate this kind of cognitive bias. We have the emergence of a new virus, then a completely new pandemic situation, with completely novel cascading impacts. We are thus in the perfect situation to see outdated inner cognitive models wreck havoc on a situation that is already catastrophic.
Thus, we absolutely need to apply all methodologies that help us overcome the use of outdated models. Explicit modelling and methodologies of strategic foresight and warning including monitoring are crucial here.
We must all learn to handle uncertainty
Strategic foresight and notably scenarios, furthermore, can help us handling uncertainties when they remain.
Indeed, modeling and scenario-building are the methodological tools epidemiologists use (e.g. for a recent and very influential study, Imperial College COVID-19 Response Team, Impact of non-pharmaceutical interventions (NPIs) to reduce COVID19 mortality and healthcare demand, 16 March 2020). And we, as social scientists, risk managers and decision-makers, must also follow suit and use this approach.
Meanwhile, the range of responses we deploy must also, ideally, be as quick and flexible as possible. This is challenging, but this is possible.
Even small businesses can do it. One way forward, in terms of capabilities, could be to mutualise some parts of the work, for example within chambers of commerce, or professional associations.
Even individuals can and should do it. Indeed, in a pandemic, they are those who are first on the front line. The need to care and protect first and foremost the medical staff is constantly highlighted. This is, of course, indispensable. Each profession that participates in activities crucial for survival is key.
Yet, alongside them as professional groups, those who fight on the front line are each and every individual, their body and their understanding of the situation. They are those who will stop or not the contagion. And they are those who will win against the virus or not.
Framing our issue – surviving then reconstructing
Rediscovering survival matters
We have moved from a normal type of life and system to an emergency one, where only survival matters.
The reasons for this move, despite the many conspiracy theories and denials of all sorts spreading, is grounded in the risks entailed by what we called crude worst case baseline scenarios. This is the epidemiological approach where overall possible fatalities are estimated, before scenarios to handle the pandemic start being modelled (e.g. Imperial College COVID-19 Response Team, Impact of non-pharmaceutical interventions (NPIs) to reduce COVID19 mortality and healthcare demand, 16 March 2020). We thus shall not come back to this point here.
Thus, we have become aware again of the importance of survival as prime motivation. We are living the essence of what politics is really about: human beings are organised in society to survive, and the fundamental mission of political authorities is to ensure their survival and security (e.g. What is Political Risk? and related bibliography). Most people had forgotten these essentials, but the pandemic reminded us powerfully and pitilessly of these fundamentals.
If you think about it, what we are all living through is absolutely extra-ordinary. Country after country, in a couple of days, according to cases, we went from a business as usual state (for those who were not paying attention to the world) to complete confinement, end of economic supremacy, closed borders, end of freedom, end of “fun”. And 168 countries face, one after the other, the same ordeal in a couple of months. And we see it and communicate about it across vast distances. This is completely new too.
Destruction and reconstruction
Meanwhile, and as a result, the usual pre-COVID-19 system is being destroyed.
The scope, magnitude and depth of the destruction will depend upon how long the COVID-19 state of emergency system will last, upon the lethality and the amount of sufferings the pandemic will inflict on the population. It will also depend, relatedly, on the way the pandemic and the COVID-19 emergency system are handled and the resilience of the pre-COVID system.
The reconstruction, in turn, will depend upon what “part” of the pre-COVID-19 world as a socio-ideological and political system has been destroyed and how this destruction was carried out. It will be determined by the amount of damages and sheer destructions the pandemic directly caused. The state of the various actors at the end of the pandemic, i.e strength, capabilities, intentions, trauma etc., will also, and as strongly, influence reconstruction.
The case of face mask shortages
For example, what the populations and their ruling authorities live, the intractable hurdles and fear they face, will remain as a burning mark in their memories. Those will certainly strongly shape their future decisions and actions.
For instance, the whole of Europe and the U.S. face an incredible shortage of face masks (e.g. Yanqiu Rachel Zhou, “The global effort to tackle the coronavirus face mask shortage“, The Conversation, 17 March 2020; Keith Bradsher and Liz Alderman, “The World Needs Masks. China Makes Them — But Has Been Hoarding Them“, 13 March 2020, updated 16 March, The New York Times).
This results from past mismanagement and from intense outsourcing of face mask manufacturing capabilities, notably to China that produces half of them (Ibid.; Fabien Magnenou, “Coronavirus : pourquoi la France manque-t-elle de masques de protection respiratoire ?“, France Info, 19 March 2020).
Consequently, the non-producers must wait on others’, and notably China, good will and benevolence and gifts. They must wait until exports become available again.
Thus, new production capabilities must be recreated from scratch, in a hurry, thanks to imagination, courage and good will, while the know-how must be reinvented. Adequate materials may lack. At the beginning, the resulting products may not be as safe as needed (e.g. Juliette Garnier, “Coronavirus : mobilisation générale pour fabriquer des masques en tissu“, Le Monde, 17 March 2020).
In the meantime, the contagion spreads and people die. On the bright side, innovation and new ways to produce will emerge from this struggle for face masks.
Yet, the stress and the fatalities and the fear will certainly not be forgotten in our lifetime and maybe for generations. As a result, it is very likely that major outsourcing to China or elsewhere is over, especially for goods that could be of critical importance.
To come back to our main question, we are thus faced with a twin task. We must foresee the near future to be able to survive while, in the same time, identifying various scenarios of destruction and nascent reconstruction. Then, building from and upon this first layer, we must foresee possible ways to reconstruct.
Looking for a first structure for our set of scenarios
On the importance of time
As a preamble, we need to stress a supplementary challenge we face when building the architecture of our set of scenarios for the COVID-19 pandemic.
We need to introduce a relatively precise timeframe. Indeed, the length of time during which the pandemic will last, as well as the timing and duration of measures taken does matter. This is obvious when looking at epidemiological studies, which will be one of the main materials upon which we shall build (e.g. Imperial College COVID-19 Response Team, Ibid.; Joseph T Wu et al. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study, The Lancet, 31 January 2020).
Key critical factors: vaccine and antiviral prophylaxis and treatment
The first factor that determines all the others is the existence – or rather in our case the non-existence – of vaccine and/or antiviral prophylaxis and treatment. Once either vaccine or treatment or both are viable, then a second key question is their availability in sufficient quantity where they are needed. Finally, we have the operationalisation of mass vaccination and/or treatment. These elements are absolutely critical.*
Indeed, once a vaccine will have become widely available and will have immunised the population, then the pandemic will end. In the case of treatments, we shall have potentially more variations and shades, but, fundamentally, the way the factor operates will likely be similar. We shall refine this statement after analysis.
The scientific effort to identify possible vaccines candidates and antiviral prophylaxis and treatment is considerable. This could take place thanks notably to very early Chinese efforts to “sequence the genetic material of Sars-CoV-2” and willingness to share it as quickly as possible (e.g. Wu, F., Zhao, S., Yu, B. et al. A new coronavirus associated with human respiratory disease in China. Nature 579, 265–269 (2020), 3 February 2020; updated GenBank “SARS-CoV-2 (Severe acute respiratory syndrome coronavirus 2) Sequences“; Laura Spinney, “When will a coronavirus vaccine be ready?“, The Guardian, 13 March 2020).
We should, however, note – for the next pandemic – that time has been lost those last years and notably since the SARS 2003 epidemic. Indeed, “medication against coronaviruses” were not included in the progress made over the last 25 years in antiviral medication (interview of Matthias Götte, a biochemist and viral researcher from Hamburg in Kerstin Kullmann und Veronika Hackenbroch, “The Urgent Search for a Cure for COVID-19“, Der Spiegel, 13 March 2020).
Vaccine
Discovery matters
Various companies, universities and research laboratories would currently be exploring between 15 (Pang et al., Feb 2020, see table on vaccines) and 35 vaccine candidates of various types (Laura Spinney, Ibid.). They are all in the early stages of the overall process (Ibid.; John Hodgson, “The pandemic pipeline“, Nature, 20 March 2020). By 15 April, more than 70 vaccine candidates would be explored, five being at the preliminary trials’ stage (Christine Soares, “The lifeline pipeline“, Reuters, 13 April 2020).
For example, human trials have already started for U.S. Moderna Therapeutics’ candidate vaccine (Michelle Roberts, “Coronavirus: US volunteers test first vaccine“, BBC, 17 March 2020). In that case the animal trials have even been skipped (Ibid.). Other human trials will start in April 2020 (Spinney, Ibid.). French Sanofi is also working on a candidate vaccine (see below).
Hodgson states that another candidate vaccine, developed by Singapore, would be at the manufacturing stage (Hodgson, Ibid.). This is probably an editing mistake, because after verification, the vaccine, developed with the Company Arcturus has not yet entered clinical trials. They expect to start phase 1 of clinical trials “in the third quarter of the year” and to complete it at the end of 2020 or beginning of 2021 (Joyce Teo, “Countries, including Singapore, in race to develop vaccine“, Straits Times, 25 March 2020). Thus, Singapore and Arcturus are nowhere near the manufacturing stage. However, Arcturus suggests that their manufacturing process will be quicker than for other vaccines (Arcturus website ibid.).
Chinese CanSino Biologics Inc. has also started conducting first phase clinical trial, which should last until December 2020 (China embarks on clinical trial for virus vaccine, The Star, 22 March 2020).
Manufacturing vaccin doses matters too
In general, scientific studies estimate that we are at best between 10 and 18 months away from a vaccine (e.g. interviews in Spinney, Ibid.; Helen Stillwell, “SARS-CoV-2 – The vaccine landscape“, Virology Blog; 11 March 2020; Roy M Anderson et al., “How will country-based mitigation measures influence the course of the COVID-19 epidemic?” – The Lancet – Published online March 09, 2020). These studies however rarely mention which phase of the vaccination process is included in these 10 to 18 months.
The director of the U.S. National Institute of Allergy and Infectious Diseases (N.I.A.I.D.) assesses that “the earliest it [a vaccine] would be deployable is in a year to a year and a half,” which would tend to imply that it has been manufactured by then (Carolyn Kormann, “How Long Will It Take to Develop a Coronavirus Vaccine?“, The New Yorker, 8 March 2020).
For its part, the global head of vaccine research and development of Sanofi estimates that, at best “a vaccine could be fully ready for licensure in a year and a half.” (Ibid.) In that case, this means that the time to manufacture doses is not included in the year and a half. This may sound logical as without the composition of the vaccine, it may be hard to assess the time needed to produce it and in which quantities.
As far as estimates of manufactured doses are concerned, the firm Inovio, for example has as target 1 million doses by the end of 2020 (Tarryn Mento, “Inovio Pharamaceuticals Fast-Tracking Human Trials, Working On 1 Million Doses Of Coronavirus Vaccine“, KPBS, 20 March 2020). This is only a target as its production capability by end of January 2020 was 100.000 doses a year (Jon Cohen, “Scientists are moving at record speed to create new coronavirus vaccines—but they may come too late“, Science, Jan. 27, 2020).
Moderna could produce at best 100 million doses a year, but would use all its production capability for it (Cohen, ibid.). For another candidate vaccine, “the Queensland team says it could make 200,000 doses in 6 months” (Cohen, Ibid,).
Sanofi, for the U.S., “has the established capacity and infrastructure to make up to 600 million doses in two existing facilities based in New York and Pennsylvania, without compromising the supply of vaccines for other illnesses, including influenza” (Sanofi, “Sanofi Mobilizes to Develop a Vaccine against COVID-19“, 23 march 2020). Meanwhile, on 23 March 2020, Sanofi confirmed its timeline: “We estimate that we will have a vaccine candidate available for in vitro testing within six months and potentially enter clinical trials within a year and a half” (Sanofi, “Sanofi’s Response in the Fight against COVID-19“, 23 march 2020).
In he meantime, the 2017 created Coalition for Epidemic Preparedness Innovation (CEPI) is building up its capacity to produce “multiple millions of doses available within 12–18 months” (Hodgson, Ibid.).
China vaccines manufacturers also now have massive capabilities to produce vaccines. In 2018, Yaming Zheng et al. estimated that China produced annually 700 million vaccine doses (The landscape of vaccines in China: history, classification, supply, and price. BMC Infect Dis).
Global estimates of future production of vaccine doses remain quite elusive and will need to be handled through scenarios, waiting for further research.
How long could the emergency or survival period last? A first estimate
This first open source brief review gives us the guidelines to conduct further in-depth study and to define the monitoring that will need to take place. Indeed, we now have the material to identify at least a first batch of indicators to monitor to follow the situation on the ground.
Meanwhile, each uncertainty related to the “vaccine factor” will create a sub-branch in our scenario tree. In other words, in the following paragraphs, each time I’ll make an assumption and use a word such as “imagine” or “if”, this means that we are dealing with sub-branches and sub-scenarios.
Waiting for a finalised architecture for our scenario tree, we can already roughly outline a very optimistic scenario. This is a scenario where at least one current candidate vaccine goes successfully through all the trials, in 12 months. This brings us, for the start of the manufacturing process to March 2021.
Here, we must remember that Singapore and those using a technology similar to Arcturus could produce more quickly the vaccines. However, the clinical trials must be successful first.
Now, a 2018 presentation by the chair of RA WG at Vaccines Europe (a specialised vaccines group within the European Federation of Pharmaceutical Industries and Associations (EFPIA), the professional association of the pharmaceutical industry in Europe) gives 24 months for the overall vaccine manufacturing process, up to distribution (slide 6 – see below).
Let us imagine – but further sub-scenarios will be necessary here actually – that efforts will be made and succeed at speeding up this process and reduce it to 20 months. This brings us to November 2022. And then a mass vaccination campaign must start. We shall leave this part aside for now, but it is nonetheless important to underline that a mass immunization campaign is not a small endeavour (e.g. WHO “Aide Mémoire – To ensure the efficiency and safety of mass immunization campaigns with injectable vaccines“)
Here, we must wonder about the number of doses that need to be injected for immunization. We must wonder about the length of the immunization. If ever the SARS-CoV-2 mutates and changes every year, as with the flu, or if it does not, we have different scenarios in front of us.
In the best of case, we can imagine that only one dose needs to be injected, and that immunization will last for years. We may also assume that herd immunity can be reached with only 70% of the population receiving the vaccine (a crude estimate of what is considered as necessary for the influenza, see, Kenneth A.McLean, Shoshanna Goldin, Claudia Nannei, Erin Sparrow, Guido Torelli, “The 2015 global production capacity of seasonal and pandemic influenza vaccine“,Vaccine, Volume 34, Issue 45, 26 October 2016, pp. 5410-5413; “Community Protection“, table in Paul E.M. Fine, … W. John Edmunds, in Plotkin’s Vaccines (Seventh Edition), 2018).
In these conditions, as a crude approximation, we may need a production of 70% x 7,7 billion = 5,39 billion doses to immunize the world against the SARS-CoV-2.
Various scenarios of collaboration and possible international tensions related to this production may thus also need to be built.
In any case the evolution of the vaccine process must be closely anticipated and monitored for action as no nation and no government will be there able to afford a situation looking like what happened with face masks.
As a conclusion, a first crude estimate of a best case scenario for the vaccine suggests that we shall have to wait until winter 2022-2023. This assessment includes many unknowns that we must handle through scenarios, monitoring and ongoing revision. Furthermore, completely unpredictable events, can also occur, such as a mutation of the virus towards less lethality for example, to be optimistic.
We have progressed into building the overall structure of our scenario tree. We also have a timeframe. Meanwhile, this timeframe also tells us that we cannot sit and wait for a vaccine. At this very early stage of our work, the years ahead for the surviving system or surviving stage, will likely need to include a vast array of imaginative solutions, mixing isolation and lock down, new ways of organisation and production, improved personal protection, new technological capabilities such as artificial intelligence, and, critically, antiviral prophylaxis and treatment.
We shall look next at main potential antiviral treatment including the chloroquine that generates so much hope (e.g. Zhonghua Jie He He Hu Xi Za Zhi. 2020 Mar 12;43(3):185-188. doi: 10.3760/cma.j.issn.1001-0939.2020.03.009 “Expert consensus on chloroquine phosphate for the treatment of novel coronavirus pneumonia”; Jianjun Gao, Zhenxue Tian, Xu Yang, “Breakthrough: Chloroquine phosphate has shown apparent efficacy in treatment of COVID-19 associated pneumonia in clinical studies“, BioScience Trends, 2020, Volume 14, Issue 1, Pages 72-73, Released March 16, 2020, [Advance publication] Released February 19, 2020).
*For vaccines, the 2017 created Coalition for Epidemic Preparedness Innovation (CEPI) identifies five steps: Discovery, Development /licensure, Manufacture, Delivery/stockpiling, Last mile.
Further detailed bibliography
Anderson, Roy M, Hans Heesterbeek, Don Klinkenberg, T Déirdre Hollingsworth, “How will country-based mitigation measures influence the course of the COVID-19 epidemic?” – The Lancet – Published online March 09, 2020
Pang J, Wang MX, Ang IYH, Tan, SHX, Lewis RF, Chen, JI, Gutierrez RA, Gwee SXW, Chua PEY, Yan Q, Ng XY, Yap RKS, Tan HY, Teo YY, Tan CC, Cook AR, Yap JCH, Hsu LY, “Potential Rapid Diagnostics, Vaccine Therapeutics for 2019 Novel Coronavirus (2019-nCoV): A Systematic Review,” J. Clin. Med. (2020) 9(3), doi: 10.3390/jcm9030623 (received 13 February 2020 ).
Wu, F., Zhao, S., Yu, B. et al. A new coronavirus associated with human respiratory disease in China. Nature 579, 265–269 (2020), 3 February 2020. https://doi.org/10.1038/s41586-020-2008-3.
Thevarajan, I., Nguyen, T.H.O., Koutsakos, M. et al. Breadth of concomitant immune responses prior to patient recovery: a case report of non-severe COVID-19. Nat Med (2020). https://doi.org/10.1038/s41591-020-0819-2
Zheng, Y., Rodewald, L., Yang, J. et al. The landscape of vaccines in China: history, classification, supply, and price. BMC Infect Dis18, 502 (2018). https://doi.org/10.1186/s12879-018-3422-0
Featured image: Image by Gerd Altmann from Pixabay, Public Domain